5 Ways HIV Develops Resistance to RTIs
Understanding HIV Resistance to Reverse Transcriptase Inhibitors (RTIs)

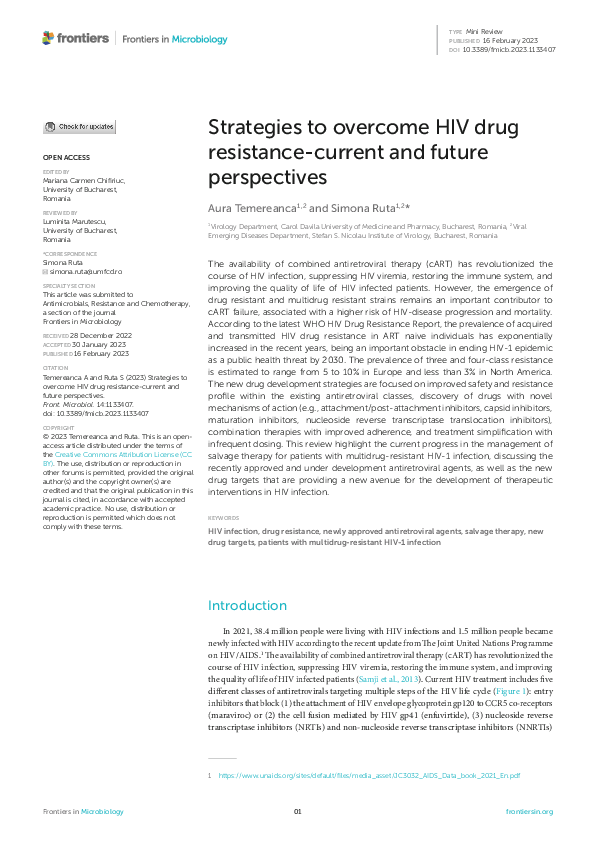
HIV, or Human Immunodeficiency Virus, is a complex and constantly evolving pathogen that has developed various mechanisms to evade the host’s immune system and resist antiretroviral therapies, including Reverse Transcriptase Inhibitors (RTIs). RTIs, such as nucleoside reverse transcriptase inhibitors (NRTIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs), are a crucial component of Highly Active Antiretroviral Therapy (HAART) regimens, which have revolutionized the management of HIV infection. However, the emergence of RTI-resistant HIV variants poses a significant challenge to effective treatment and highlights the need for ongoing research into new therapeutic strategies.
How HIV Develops Resistance to RTIs

HIV develops resistance to RTIs through a combination of genetic mutations, recombination, and selection pressures exerted by the antiretroviral agents themselves. Here are five key ways in which HIV can evade the effects of RTIs:
1. Genetic Mutations in the Reverse Transcriptase Gene

HIV’s genetic material, consisting of two copies of single-stranded RNA, is prone to errors during replication. These errors can result in mutations in the reverse transcriptase gene, which codes for the enzyme responsible for converting viral RNA into DNA. Some of these mutations can confer resistance to RTIs by altering the shape of the reverse transcriptase enzyme or reducing its affinity for the inhibitors.
Examples of mutations that confer resistance to RTIs:
- M184V/I mutation, which confers resistance to lamivudine (3TC) and emtricitabine (FTC)
- K65R mutation, which confers resistance to tenofovir (TDF), didanosine (ddI), and abacavir (ABC)
2. Development of Novel RNA Secondary Structures
HIV’s RNA genome can form complex secondary structures, such as stem-loops and pseudoknots, which play a crucial role in viral replication and packaging. Some mutations can alter these secondary structures, allowing the virus to evade RTI inhibition.
Examples of RNA secondary structures involved in RTI resistance:
- The TAR (trans-activation response) element, which is involved in viral transcription and can be affected by mutations that confer resistance to NNRTIs
3. Recombination and Genetic Variation
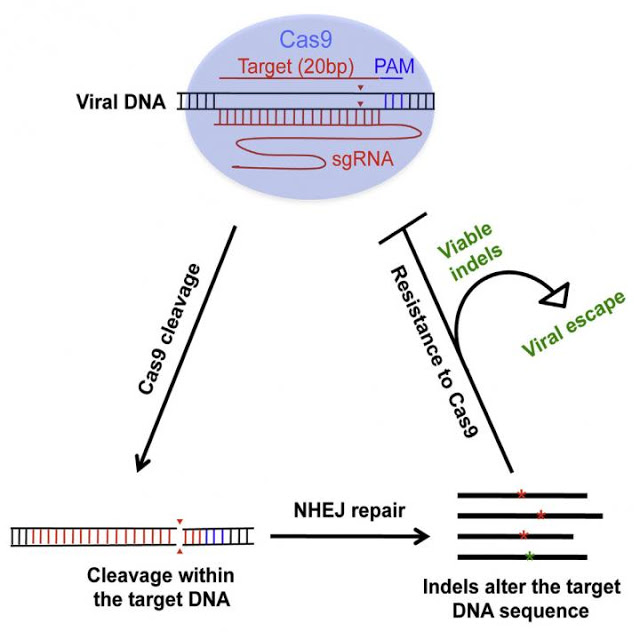
HIV is a highly recombinogenic virus, meaning that it can readily exchange genetic material with other viruses during replication. This recombination can lead to the creation of novel viral variants with altered RTI susceptibility.
Factors that contribute to recombination and genetic variation:
- High error rate of the reverse transcriptase enzyme
- Frequent co-infection with multiple HIV strains
- Antiretroviral therapy, which can exert selective pressure on the virus to evolve resistance
4. Epigenetic Modifications and Chromatin Structure

Epigenetic modifications, such as DNA methylation and histone acetylation, can affect chromatin structure and gene expression. HIV has been shown to exploit these mechanisms to evade RTI inhibition.
Examples of epigenetic modifications involved in RTI resistance:
- DNA methylation of the HIV promoter region, which can reduce viral transcription and replication
- Histone modifications that affect chromatin structure and RTI access to the viral genome
5. Cell-to-Cell Transmission and Viral Sanctuaries

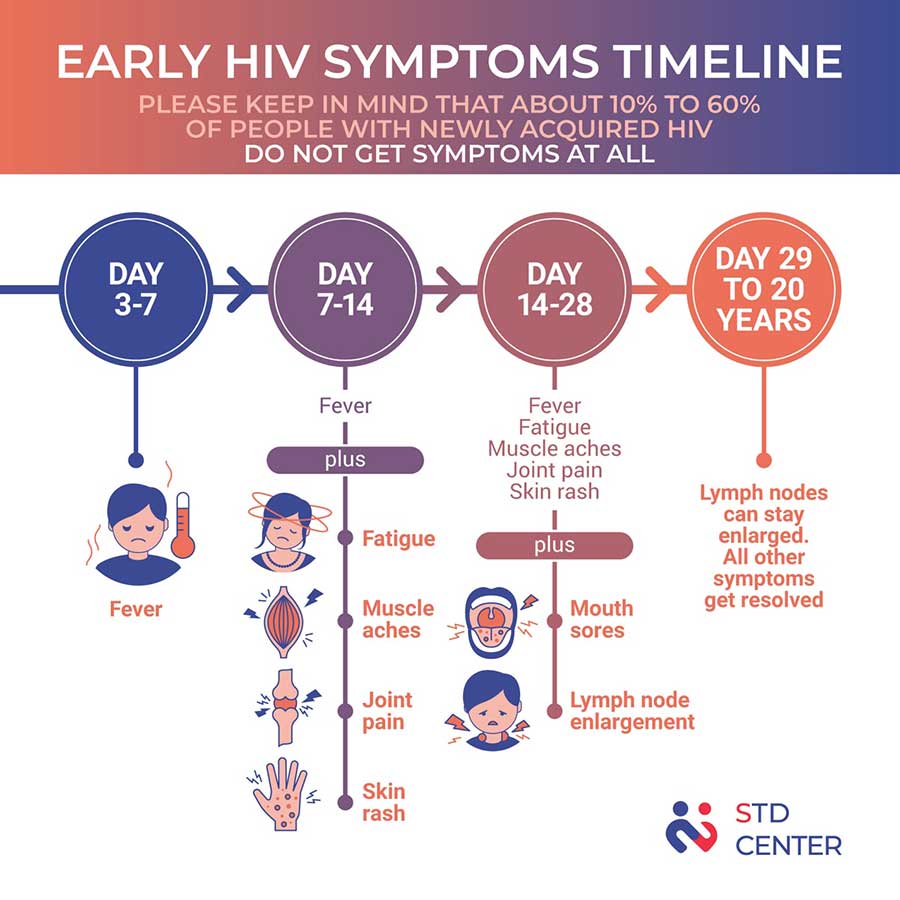
HIV can spread from cell to cell through direct contact, a process known as cell-to-cell transmission. This mode of transmission can facilitate the spread of resistant viruses and allow them to evade the effects of RTIs.
Factors that contribute to cell-to-cell transmission and viral sanctuaries:
- Direct cell-to-cell contact between infected and uninfected cells
- Presence of viral sanctuaries, such as lymphoid tissues and the central nervous system, where the virus can replicate and evade antiretroviral agents
💡 Note: The development of RTI resistance is a complex and multifaceted process, and these five mechanisms are not mutually exclusive. Understanding the interplay between these factors is crucial for the design of effective antiretroviral therapies and treatment strategies.
In summary, HIV develops resistance to RTIs through a combination of genetic mutations, recombination, and selection pressures exerted by antiretroviral agents. Understanding these mechanisms is essential for the development of novel therapeutic strategies and for optimizing treatment outcomes in patients with HIV infection.
What is the main mechanism of HIV resistance to RTIs?

+
The main mechanism of HIV resistance to RTIs is through genetic mutations in the reverse transcriptase gene, which can alter the shape of the reverse transcriptase enzyme or reduce its affinity for the inhibitors.
What are some examples of mutations that confer resistance to RTIs?
+
Examples of mutations that confer resistance to RTIs include the M184V/I mutation, which confers resistance to lamivudine (3TC) and emtricitabine (FTC), and the K65R mutation, which confers resistance to tenofovir (TDF), didanosine (ddI), and abacavir (ABC).
How does recombination contribute to RTI resistance?
+
Recombination can lead to the creation of novel viral variants with altered RTI susceptibility, as HIV can readily exchange genetic material with other viruses during replication.